By John Pickard
For many people who are not of a religious persuasion, including yours truly, Christmas is still a time for eating good food and imbibing nice drinks. But at the risk of being labelled a killjoy, is it not worth pondering a little on the interface between politics and food and the relationship of both of these to health?
The two biggest threats to general public health in the UK, and in the West in general, are diabetes and obesity, which are linked to each other and are associated with coronary heart disease, strokes, high blood pressure, inflammatory conditions and many other adverse medical effects.
According to the website of the charity Diabetes-UK, over four million people in the UK were living with a diagnosis of some type of diabetes in 2021. They estimated that there were an additional 850,000 living with type 2 diabetes that has gone undiagnosed.Cases of diabetes have doubled in the last 15 years.
“We estimate” they say, “that there are also more than 13.6 million people at increased risk of type 2 diabetes in the UK. At this rate, we predict that the number of people with diabetes, including the undiagnosed population, is expected to rise to 5.5 million by 2030”.
Diet is the main determinant of type 2 diabetes
Globally, it is estimated that over 450 million people have type 2 diabetes, around 6% of the world population. “More than a million deaths were attributed to this condition in 2017 alone, ranking it as the ninth leading cause of mortality. This is an alarming rise when compared with 1990, when type 2 diabetes was ranked as the eighteenth leading cause of deaths”. (National Centre for Biotechnical Information). In Western countries, the cost of diabetes and obesity to health services is immense.
There are many factors that affect a person’s risk of having type 2 diabetes, including age, family history and ethnicity. But the most important from a social point of view is diet. Contrary to what is commonly believed – and such ideas can still be found on the websites of some charities – obesity is not a cause of type 2 diabetes but is a result of a metabolic dysfunction (more of which later). Although there is a close association between the two, modern research shows that metabolic dysfunction, of which diabetes can be one part, causes obesity.
For a long time, we were told that the growing epidemic of coronary heart disease (CHD) – also associated with obesity – was due to too much fat in the diet. Many of us were brought up to look at the amount of fat in food and to judge it accordingly. In fact, as we now know, fat is not the main enemy of health, it is sugar. The first major and very influential scientific reviews that linked coronary heart disease to diet were skewed by the influence of the sugar corporations, who in many cases even paid for the research.
For years the finger of guilt was made to point at fat
The website foodnavigator.com published a report showing that in the 1960s and 1970s, the US sugar lobby paid for influential research that played down the link between CHD and sugar and instead pointed the finger of guilt at fat. The Journal of the American Medical Association published a paper in November 2016 that is worth quoting some of this at length:
“The Sugar Research Foundation (SRF) sponsored its first CHD research project in 1965, a literature review published in the New England Journal of Medicine, which singled out fat and cholesterol as the dietary causes of CHD and downplayed evidence that sucrose [sugar] consumption was also a risk factor. The SRF set the review’s objective, contributed articles for inclusion, and received drafts. The SRF’s funding and role was not disclosed. Together with other recent analyses of sugar industry documents, our findings suggest the industry sponsored a research program in the 1960s and 1970s that successfully cast doubt about the hazards of sucrose while promoting fat as the dietary culprit in CHD”.
Excessive fat in the diet is not a good idea, but fat per se is not the cause of the obesity/diabetes epidemic. That doesn’t stop shops selling everything ‘low fat’ because it is still perceived as a good selling point, so low-fat yoghurts, milk, cheese and just about everything can still be found in supermarkets. It is hard to find any ‘full fat’ products on some shelves.
The manufacturers and retailers are doubly pleased – they have a good selling point (irrespective of the science) and the fat which has been ‘skimmed’ from whole milk can be used to make and sell another product. Hey presto! – two lots of profit instead of one.
But as we now know, and is becoming clearer with modern research, obesity, coronary heart disease, type 2 diabetes and other manifestations of metabolic dysfunction are caused by excessive carbohydrate in the diet and specifically sugar.
How insulin interacts with glucose
At this point, we need to look at the science behind carbohydrate digestion and absorption into the body. Plant-based starch is the chief source of carbohydrate energy in modern diets and on a molecular level starch is composed of giant chains of glucose molecules linked together. (See diagram below)
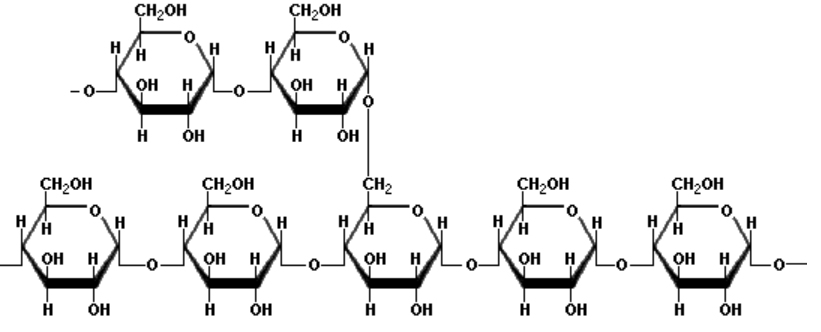
All your digestive system has to do is to break the links in the chain and the glucose goes freely into the blood, to be transported around the body, where it is the principle source of energy for the cells. When the level of glucose in the bloodstream begins to rise, a hormone – insulin – is released by the pancreas to promote the absorption of glucose by the body cells, where it can be used or stored in the form of glycogen, a molecule also made up of chains of glucose similar to starch (hence sometimes called ‘animal starch’).
Insulin therefore reduces the level of glucose in the blood, at the same time that it is making it available to the cells. If more glucose is needed than is already in the bloodstream, for example when muscles begin to exercise, then the stored glycogen can be ‘mobilised’ to release glucose back into the bloodstream.
The problem is that in the modern diet, one could say that there is a too great a supply of ‘neat’ or ‘pure’ carbohydrate available in many foods, like bread, rice and pasta. Starch is much more readily available, and in a very concentrated form, than it was hundreds of thousands of years ago, when the human digestive system was evolving. Processed carbohydrates, like non-wholemeal bread and rice, purify the starch even more. The modern carb-rich diet, in a nutshell, causes an ‘over-use’ of the insulin response.
Our metabolic system evolved with a primitive diet
We say this is a modern issue because human metabolism (as it is now) completed its biological evolution around 120,000 years ago, give or take a few thousand years, and that evolution pre-dates modern diets. Our biological evolution has not kept pace with our social evolution, at least in terms of diet.
During the years of its development, as it evolved, the human digestive system would have mostly dealt with plant material, much of it raw: nuts, seeds, vegetable roots, leaves and fruit. Meat also supplemented these vegetables and meat protein was an important source of amino acids for growth and for energy.
Something like this kind of diet: a mixed-plant diet, supplemented by meat, was probably the basis of the hominid diet for hundreds of thousands of years before ‘modern’ humans evolved. There may have been occasional bounties of rich carbohydrates – like honey from a bees’ nest, or over-ripe fruit – but in general such carbohydrate-rich food would have been the exception.
At a certain point in human development, agriculture made an appearance. Plants began to be cultivated for their higher energy content and ready availability: two big advantages over foraged plants. Growing crops, therefore, meant that a surplus of food energy could be produced for the first time and that laid the basis for society to develop social classes, because some people did not need to be food producers. Cultivation of crops also led to the development of settlements, towns and cities. The rest, as they say, is history.
The interaction between biological evolution and social evolution is dialectical. As one ‘problem’ is resolved – the ready availability of food energy – another contradiction takes its place: that between a metabolic system adapted to a very varied, largely plant-based diet, and a diet with a smaller number of carbohydrate-rich foods. Human metabolism has not changed – even to this day – even though societal developments and diets have.
A ‘calorie is not a calorie’
In ‘primitive’ humans, where most energy came in the form of nuts, fruits, vegetables and seeds, less insulin was required to make the cells take up glucose and the pancreas which makes the insulin was not overtaxed in making insulin. Apart from anything else, the ‘mixture’ of foods eaten would have meant that glucose was released into the bloodstream in a more measured way and the insulin could do its job putting glucose into the cells.
As an aside, the idea that ‘a calorie is a calorie’ is wrong, because the glucose in some foods is released almost immediately, causing blood glucose spikes, whereas in others it is released over a longer period of time (or not at all) because it is ‘bound’ up with other chemicals or to dietary fibre. Even a modern carbohydrate-rich diet would be healthier, for example, if the carbs were mixed with sufficient quantities of fresh fruit and vegetables. In addition, different foods interact upon each other to reduce (or speed up) glucose release.
Coming to modern diets, a large amount of glucose is available from ‘pure’ or ‘refined’ carbohydrates, and as a result the insulin response has a bigger job to do, because there is so much glucose in the blood which needs to be dumped into cells. White table sugar, for example, is nearly 100% pure sucrose and wouldn’t occur in such purity anywhere in nature, yet it is ubiquitous in modern processed foods.
Frequent spikes in blood glucose cause insulin resistance
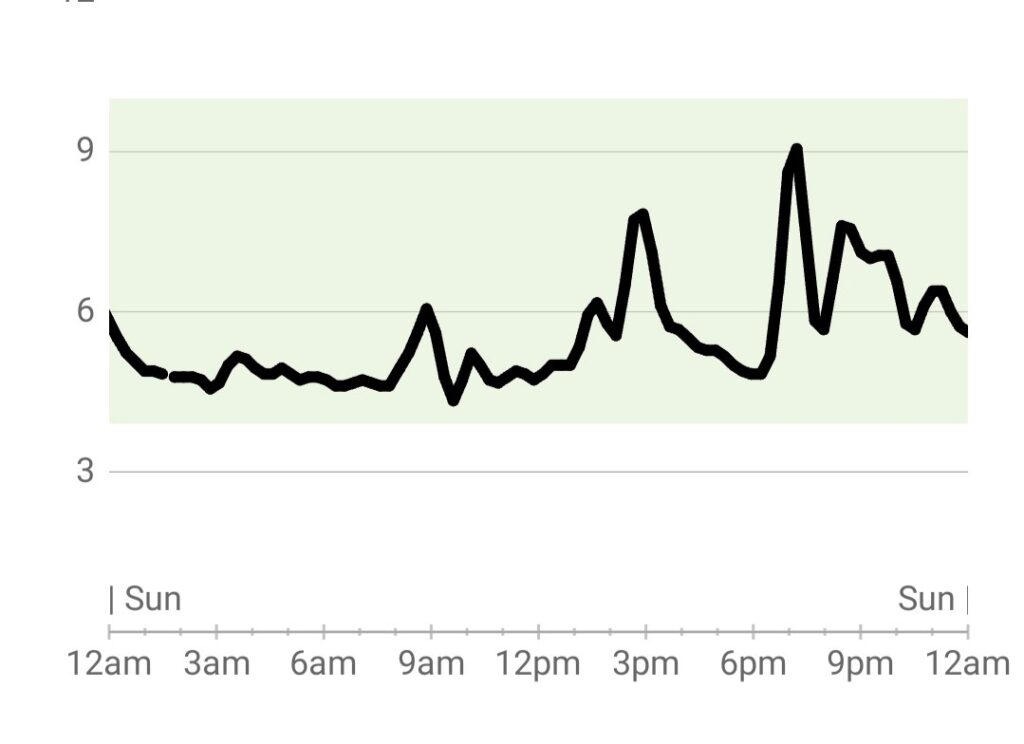
Imagine a modern meal, including refined carbohydrate and (more than likely) a portion of sugar. Glucose is released extremely quickly into the bloodstream and if the insulin cannot cope immediately, there is a ‘spike’ in blood glucose. Up to a point this is normal, and the graph inset below shows real-time peaks corresponding to three meals, as shown by a blood glucose sensor attached to a relatively healthy person.
So with a lot of unrefined carbohydrate or sweet foods (see next part, for how sugar works) blood glucose can shoot up very suddenly – and to a high level – and the insulin has to try to deal with this to an enhanced degree. Sometimes the heightened impact of the insulin can then produce a rapid collapse in blood glucose level, inducing dizziness, sweating and other unpleasant effects.
The problem is this: regular and frequent high glucose spikes, promoting surges of insulin, can eventually create insulin resistance in the bodies’ cells and that is when there is dysfunction, nowadays generalised by scientists in the term metabolic syndrome. A feature of metabolic syndrome can be poor or erratic control of blood glucose and diabetes. Type 2 diabetes is specifically linked to a level of blood glucose that is too high because insulin resistance means it fails to get the glucose into the cells.
Metabolic syndrome will also lead to obesity in most cases, because the insulin resistance of those cells that fail to take up glucose is counteracted by the ‘wrong’ cells storing glucose in the form of triglycerides (fats). This storage of fat takes place inside the body and around vital organs, where it is dangerous, rather than under the skin on the surface of the body.
What exacerbates the problem is that frequent and high glucose spikes will also lead to a feeling of hunger. Hormones controlling the feeling of ‘hunger’ get out of synch. Leptin, is the hormone that tells our brains we are ‘full’ but it is suppressed by too much insulin and another hormone, ghrelin, which tells the brain that we are ‘hungry’ takes over. Hormone imbalance, therefore, really can lead people to eat more when they don’t really need to, further exacerbating the problem – especially if they are eating the wrong kinds of food.
In the next section, we will look at the worst carbohydrate from a health point of view: sugar.